|
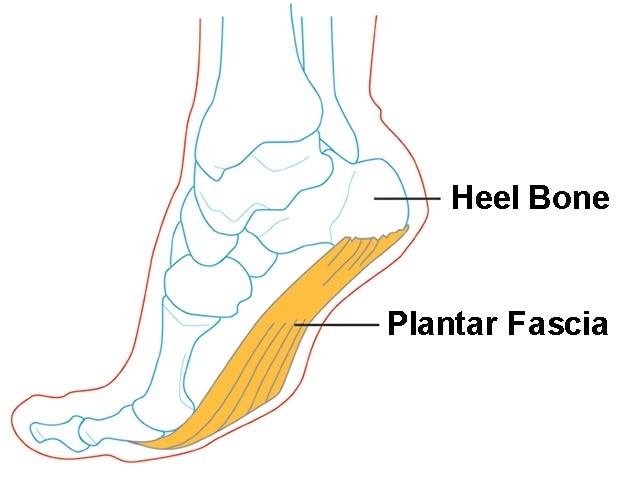
Plantar fasciopathy (also known as plantar fasciitis) is an overuse condition of the plantar fascia at its attachment to the calcaneus (heel bone). It is the most common cause of plantar heel pain, which has an estimated prevalence of 4-7% of the population.
Anatomy The plantar fascia is a strong band of tissue (like a ligament) that stretches from your heel bone to your middle foot bones. It supports the arch of your foot and also acts as a shock absorber in your foot. Common Causes/Risk Factors Plantar fasciopathy commonly affects very physically active people (e.g. runners) or people with high amounts of standing occupations work (who may also have a high BMI). Only one true prospective study has investigated risk factors for plantar fasciopathy. The study was conducted in a cohort of 166 runners followed over 5 years. The study found the overall incidence of plantar fasciopathy over the 5 year period to be 31%. Four risk factors that were significantly associated with an increased risk of plantar fasciopathy were:
Other risk factors for plantar fasciopathy include:
Signs and symptoms Pain is usually felt on the underside of the heel, and is often most intense with the first steps of the day or after rest. It is commonly associated with long periods of weight bearing or sudden changes in weight bearing or activity. You may experience:
What about Scans or X-rays? If a patient has the classic history and examination findings and there is no other suggestion of a ‘red flag’ then medical imaging or other investigations are not indicated. Further investigation is recommended if:
Blood tests may be warranted to rule out inflammatory arthritis, which can cause symptoms in the heels, although frequently symptoms will be more widespread. The primary imaging modalities that are useful include plain radiographs (X-rays), ultrasound or MRI. What about a Heel Spur? X-rays may sometimes show a heel spur; however, heel spurs are also common in people without heel pain, and the presence of a spur does not indicate that this is the cause of the pain. X-rays of both feet are useful as they may show spurs bilaterally and allow comparison of the feet in unilateral symptoms. Treatment Treatment is often multi-faceted and generally starts with conservative interventions, modifying load and addressing any risk-factors. A physiotherapist will usually assess your biomechanics and look at all the links in the chain, from the foot right up to the hip, pelvis and core. Some authors define treatment into First, Second and Third-Tier treatment which essentially relate to short-, medium- and long-term options. The tiers also relate to the complexity, cost and invasiveness of the intervention. First Tier/Short Term Treatment Aims: minimise the aggravating activity and educate the patient about the potential causes of their heel pain. Discuss and modify training loads as appropriate.
Second Tier/Medium Term
Third Tier/Long Term
REFERENCES: Brukner P, Khan K, et al. Clinical Sports Medicine. Volume 1, Injuries. 5th Edition. 2017. McGraw Hill Education. http://sma.org.au/resources-advice/injury-fact-sheets/plantar-fasciitis/ Plantar Fasciitis Injury Fact Sheet, Sports Medicine Australia.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDavid McWilliams graduated from Macquarie University with a Doctor of Physiotherapy. He is a member of Australian Physiotherapy Association, Sports and Exercise Physiotherapy Australia, Sports Medicine Australia Archives
April 2021
Categories |